Tuesday, November 24, 2009
Design Project
Now all my posts will be on my design project page. This is just a post to forward to another blog. HAPPY SOON TO BE THANKSGIVING!
Tuesday, November 10, 2009
Front Page of Business Section Again
"Medical Industry Grumbles, but It Stands to Gain"
http://www.nytimes.com/2009/11/09/health/policy/09industry.html?scp=1&sq=the%20medical%20industry%20grumbles,%20but%20it%20stands%20to%20gain&st=cseThe front page of the business page of The New York Times once again related to the medical industry. The article was published this Monday. Millions of more Americans would gain medical coverage if the health care reform ever gets through the Senate, but that's another story. The focus of the article is that although the medical industry would gain more "paying customers" (Wilson & Abelson, 2009), it would be subject to more regulation. A graphic from the article is below.
| ||||||
 | ||||||
| ||||||
The stipulation for a registry for medical devices relates to the article published Thursday which I mentioned in my previous blog post. I think making this reform into reality will take years (if it ever happens). A registry would benefit patients and doctors.
Sunday, November 8, 2009
the US doesn't have a registry
http://www.nytimes.com/2009/11/05/business/05device.html?scp=1&sq=Costs%20Surge%20for%20Medical%20Devices,%20but%20Benefits%20Are%20Opaque%20&st=Search

An article entitled "Costs Surge for Medical Devices, but Benefits Are Opaque" made the front page of the business section of the New York Times this Thursday. I have been meaning to blog about it for a while, but decided to today. Medicare pays millions for costly devices such as implantable defibrillators, artificial joints, and other implants. The US lacks one key thing though: a registry for these devices. Other countries have medical device databases, "to provide both doctors and patients with more data about how competing products differ. In such a database, or a registry, information about a product and the surgical technique used by a doctor is recorded at the time of an implant. And then by tracking whether and when the patients return for a replacement procedure, or experience other problems, registries can show which producers’ models are failing faster than others," (Meier, 2009). Databases would make for more competition.
Medical device companies would not gain anything if there way a registry. Patients would gain better results through the use of the "best" devices. Also implantable defibrillators have battery lives of around 5 years. The article seems to conclude that these devices could be made to have longer battery lives, but companies sell more defibrillators when they have to be replaced every five years. The cell phone industry runs a similar scheme with short battery lives and planned upgrades. Should life saving devices be programmed to fail intentionally? Patients are more than consumers. Operations to replace implantable defibrillators can lead to death. The business of medical devices in the US will soon change.
| ||||||
 | ||||||
Lance Murphey/Bloomberg News A researcher at the device maker Medtronic in Memphis examining a spinal system. | ||||||
| ||||||
An article entitled "Costs Surge for Medical Devices, but Benefits Are Opaque" made the front page of the business section of the New York Times this Thursday. I have been meaning to blog about it for a while, but decided to today. Medicare pays millions for costly devices such as implantable defibrillators, artificial joints, and other implants. The US lacks one key thing though: a registry for these devices. Other countries have medical device databases, "to provide both doctors and patients with more data about how competing products differ. In such a database, or a registry, information about a product and the surgical technique used by a doctor is recorded at the time of an implant. And then by tracking whether and when the patients return for a replacement procedure, or experience other problems, registries can show which producers’ models are failing faster than others," (Meier, 2009). Databases would make for more competition.
Medical device companies would not gain anything if there way a registry. Patients would gain better results through the use of the "best" devices. Also implantable defibrillators have battery lives of around 5 years. The article seems to conclude that these devices could be made to have longer battery lives, but companies sell more defibrillators when they have to be replaced every five years. The cell phone industry runs a similar scheme with short battery lives and planned upgrades. Should life saving devices be programmed to fail intentionally? Patients are more than consumers. Operations to replace implantable defibrillators can lead to death. The business of medical devices in the US will soon change.
Thursday, November 5, 2009
actually complete
The paper is in. After researching, analyzing, diagraming, writing, and editing the research paper is done. I learned a lot about a very specific area of tissue engineering, ACL scaffolds. It is an interesting area and I see real potential for that field to expand in the coming years, as is the case with most fields related to bioengineering. I just want to have a way to estimate the success rates of this research. Will it ever be applied to a commercial implantable device, or will it just flitter away? Accepting new techonologies takes time.
As a result of the project, I learned how to read articles from scientific journals as a result of this project. A few months ago I had never read a scientifc journal articles, The Science Times in The New York Times, is not quite the same thing. It was interesting to take information from these scientific journals and translate it into something anyone could understand. The next step is the design project. I currently have zero good ideas, but we'll see what happens in the upcoming weeks.
As a result of the project, I learned how to read articles from scientific journals as a result of this project. A few months ago I had never read a scientifc journal articles, The Science Times in The New York Times, is not quite the same thing. It was interesting to take information from these scientific journals and translate it into something anyone could understand. The next step is the design project. I currently have zero good ideas, but we'll see what happens in the upcoming weeks.
Sunday, November 1, 2009
done... well almost
I just finished my first draft of the paper. It has all the sections described in the assignment. The only thing is I cannot paste a table from a PDF file into word wothout the formatting getting all messed up. I just did not put the tables in the paper, but I will try to get them in by Thursday. The tables are tables of numbers relating to braiding angle, pore size, porosity, tensile strength, maximum load, and other things. I guess having those tables are not completely necessary for the paper. But I did put in some nice diagrams from a New York Times slideshow that clearly display the knee, a torn ACL, a patellar tendon autograft, and some other things. I think it is easier to understand something when you can look at it after reading about it, rather than just reading about it. Just focusing on the one design was enough, I did not have to compare the design with PLAGA to designs with collagen and other biomaterials. Tissue-engineering is a developing field and I think that in the future some kind of ACL tissue scaffold will be used for ACL reconstruction.
Thursday, October 29, 2009
Simplicity
I am beginning to think that my machine diagram is easy to understand. My concern is that it is overly simplistic. I mean essentially the "device" I am analyzing is a tissue engineered scaffold for ACL replacement. I am focusing on one of these scaffolds which is described in an article entitled "Fiber-based tissue-engineered scaffold for ligament replacement: design considerations and in vitro evaluation." The design of this scaffold focuses on architecture, porosity, degradability, and cell source. Architecture covers the amount of surface area. While porosity also covers the amount of surface area, it additionally involves the pore diameter. Both surface area and pore diameter function to encourage the body's ability to accept the new ACL scaffold and generate new cells. PLAGA is the biodegradable material being used to create the fibers in the scaffold. It is imperative that the fibers degrade over time and the body does not treat them as foreign materials. Biocompatibility is essential. The cell source primarily focuses on the body's cellular response. This device has not been used in humans, but rabbit ACL cells as well as mouse fibroblasts were put on the scaffold under lab conditions that simulated body conditions to see the potential for cell migration and attachment. In other words, to see if more cells were generated and to see how they moved along the scaffold.
The PLAGA fibers get braided together using 3-D braiding methods in either a circular or rectangular geometry. These entwined fibers get tested on their mechanical properties such as tensile modulus, or tendency to be deformed when a force is applied, and , maximum tensile load, or the maximum force the device can take before certain areas deform due to disproportionate amount of force and stress. The scaffold had 3 regions all made of the same PLAGA fibers, but these fibers were braided at different angles. The regions were the "femoral tunnel attachment site, ligament region, and tibial tunnel attachment site" (Copper et. al., 2004). A higher angle was used at the ends that would be attached to bone, while a lower angle was used for the ligament region. Bones are not flexible like ligaments, which explains the use of the higher angle to enable healing. After writing this, I guess my device is not as simple as I thought. I think this should be a good paper.
The PLAGA fibers get braided together using 3-D braiding methods in either a circular or rectangular geometry. These entwined fibers get tested on their mechanical properties such as tensile modulus, or tendency to be deformed when a force is applied, and , maximum tensile load, or the maximum force the device can take before certain areas deform due to disproportionate amount of force and stress. The scaffold had 3 regions all made of the same PLAGA fibers, but these fibers were braided at different angles. The regions were the "femoral tunnel attachment site, ligament region, and tibial tunnel attachment site" (Copper et. al., 2004). A higher angle was used at the ends that would be attached to bone, while a lower angle was used for the ligament region. Bones are not flexible like ligaments, which explains the use of the higher angle to enable healing. After writing this, I guess my device is not as simple as I thought. I think this should be a good paper.
Sunday, October 25, 2009
how does this work: a preliminary machine diagram

(The only way I could figure out putting the diagram into the post was literally printing it out, taking a picture of it, and uploading the picture. I could not paste it from a word or powerpoint file.)
The top left to right says: Architecture, Porosity, Degradability, Cell Source; Force, Regeneration of cells (mass).
The middle left to right says: Knee; Cells (Mass) ; PLAGA fibers.
The bottom left to right says: Knee strength and stability; Body’s ability to accept new ACL scaffold and generate, Cell migration and attachment; 3-D braiding geometry, Circular or rectangular, Biomaterial of fiber, PLGA, Braiding angle, Pore diameter, Surface area.
I found creating a machine diagram for an ACL tissue scaffold quite difficult. I am wondering whether the first component should be the knee or something else. Essentially, the scaffold is just fibers twisted together. It does not really have several "components." Here's my first attempt at a machine diagram (with the knee as component one). This is subject to change if I have some moment of genius in which I discover a more appropriate component one.
The issue at hand is that my machine is more abstract than a more mechanical device like an artificial arm. I think the item being transferred for my device is cells, although it really seems like it is the potential for the regrowth of cells. I guess an exercise like this does not have one right answer. Problems sometimes have different types of solutions that can lead to the same end result. In my project that concept is at play. Different people have studied different methods of construction ACL tissue scaffolds in terms of biomaterial used, angle the material is braided at, the pore size of the fibers, and such. They all use different methods that lead to the end result of an ACL tissue scaffold. Sure the strengths may be slighltly different, but the overall solution is to create the tissue scaffold and try to minimize
 recovery time while improving the current ACL reconstruction methods used.
recovery time while improving the current ACL reconstruction methods used.
Wednesday, October 21, 2009
focus, focus, focus
So after all that reading, note taking, quoting, and searching I have come up with my final questions.
1. Why do we need to use tissue engineering for ACL scaffolding?
5. How can it be improved?
1. Why do we need to use tissue engineering for ACL scaffolding?
- background on injury rates, number of surgeries performed annually
- why does the ACL not heal on its own?
- problems with past and current methods of treatment- allograft, autograft, prosthesis- commercial ones (Carbon Fiber Prostheses, Gore Tex, Darcon, Leeds-Keio Artificial Ligament, Kennedy Ligament Augmentation)
- more specific- why do women have a higher risk of tearing their ACLs?
- Use design from "Fiber-based tissue-engineered scaffold for ligament replacement:
design considerations and in vitro evaluation
James A. Cooper a,b,c,d, Helen H. Luf, Frank K. Koe, Joseph W. Freemana,
Cato T. Laurencin a,b,c,d,*" - Polymeric fibers of polyactide-co-glycolide 10:90 (PLGA fibers)
- Biodegradable materials
- 3-D braiding technology
- Braiding geometry
- TABLE 1- effects of braiding geometry on other parameters- "Results from the porosimetry analyses of the PLAGA
circular and rectangular braided scaffolds are summarized
in Table 1. The effects of braiding geometry on the
linear density, mode pore diameter, median pore
diameter, surface area, braiding angle, and porosity of
the scaffolds can be derived from Table 1." - Braiding angle
- Advantages of this design- controlled pore diameter promote tissue infiltration throughout scaffold, custom design with 3-D braiding, 3-D braiding prevents catastrophy from one tiny break
- design from Cooper et. al.
- Surgical implant, instead of the basically 2 procedures using an autograft (remove tissue from one area and put it in ACL), only one (just put in new scaffold)
- Architecture
- Porosity
- Degradability
- Cell Source
- IDEAL "The ideal ACL replacement scaffold should be
biodegradable, porous, biocompatible, exhibit sufficient
mechanical strength, and able to promote the formation
of ligamentous tissue." from article mentioned above - 3 regions- "The objective
was to design a scaffold that provides the newly
regenerating tissue with a temporary site for cell
attachment, proliferation, and mechanical stability. As
shown in Fig. 1, the 3-D braided scaffold was comprised
of three regions: femoral tunnel attachment site,
ligament region, and tibial tunnel attachment site. The
attachment sites had high angle fiber orientation at the
bony attachment ends and lower angle fiber orientation
in the intraarticular zone. This pre-designed heterogeneity
in the grafts was aimed to promote the eventual
integration of the graft with bone tissue. The scaffold
was composed of PLAGA fiber with diameter similar to
that of type I collagen fiber." - Cell adhesion
- Cells spread across fiber
- Cell migration and attachment
- evaluating the design described in Cooper et. al.
- ultimate tensile strengths tested- "The ultimate tensile strengths ranged
from ~100 to 400 MPa" - circular geometry was stronger than rectangular - "When the same number of yarns was
used for the rectangular and circular braids the circular
braid geometry showed a significant increase in maximum
tensile load. The 3-D circular fibrous scaffold was
able to withstand tensile loads of 907N (SD7132 N),
which was greater than the level for normal human
physical activity that is estimated to range between 67
and 700N" - Table 2- Maximum loads and ultimate tensile strength
5. How can it be improved?
- keep going with design from Cooper et. al.
- optimal braiding angle, pore size, biocompatibility
- "Future studies will focus on the scaffold’s initial
mechanical properties as compared to a rabbit model
and in vitro characterization of the cellular response and
interaction with the braided tissue-engineered ligament
scaffold."
Tuesday, October 20, 2009
Useful slides on ACL
http://www.nytimes.com/slideshow/2007/08/01/health/100230Anteriorcruciateligamentrepairseries_index.html

"The anterior cruciate ligament (ACL) is a ligament in the center of the knee that prevents the shin bone (tibia) from moving forward on the thigh bone (femur)."

"If the ACL is torn, the knee joint may become unstable and affect the ability to perform work or athletic activities."

"ACL reconstruction is surgery to replace the torn ACL ligament. There are several choices of tissue to use for the new ligament, including an autograft (tissue from the patient’s own body) or an allograft (tissue from a cadaver). One of the most common autografts use part of the patellar tendon (the tendon in the front of the knee)."
-that's also the surgery I had along with repairing a medial meniscus

"The old ligament is removed using a shaver or other instruments. Bone tunnels are made to place the new ligament (patellar graft) in the knee at the site of the old ACL. Screws are commonly used to secure the graft in the bone tunnels, although other methods of fixation are used depending on the type of graft used."

"At the end of the surgery, the incisions are closed, and a dressing is applied. ACL reconstruction is usually a very successful surgery. The majority of patients will have a stable knee that does not give way after ACL reconstruction."
-really majority of patients do have a stable knee, but not like it was before as supported by statistics in other science journals
Anterior Cruciate Ligament Repair (ACL)

"The anterior cruciate ligament (ACL) is a ligament in the center of the knee that prevents the shin bone (tibia) from moving forward on the thigh bone (femur)."

"If the ACL is torn, the knee joint may become unstable and affect the ability to perform work or athletic activities."

"ACL reconstruction is surgery to replace the torn ACL ligament. There are several choices of tissue to use for the new ligament, including an autograft (tissue from the patient’s own body) or an allograft (tissue from a cadaver). One of the most common autografts use part of the patellar tendon (the tendon in the front of the knee)."
-that's also the surgery I had along with repairing a medial meniscus

"The old ligament is removed using a shaver or other instruments. Bone tunnels are made to place the new ligament (patellar graft) in the knee at the site of the old ACL. Screws are commonly used to secure the graft in the bone tunnels, although other methods of fixation are used depending on the type of graft used."

"At the end of the surgery, the incisions are closed, and a dressing is applied. ACL reconstruction is usually a very successful surgery. The majority of patients will have a stable knee that does not give way after ACL reconstruction."
-really majority of patients do have a stable knee, but not like it was before as supported by statistics in other science journals
The Uneven Playing Field
http://www.nytimes.com/2008/05/11/magazine/11Girls-t.html
This is my favorite article. It does not deal with the specifics of tissue engineering for ACLs, but it deals with the higher proportion of female ACL tears than male as well as female athletes' mentalities versus males' mentalities. The article gives a more human aspect to the issue.
This is my favorite article. It does not deal with the specifics of tissue engineering for ACLs, but it deals with the higher proportion of female ACL tears than male as well as female athletes' mentalities versus males' mentalities. The article gives a more human aspect to the issue.
- WHY NEED TISSUE ENGINEERING- "But among all the sports injuries that afflict girls and young women, A.C.L. tears, for understandable reasons, get the most attention. No other common orthopedic injury is as debilitating and disruptive in the short term — or as likely to involve serious long-term consequences. And no other injury strikes women at such markedly higher rates or terrifies them as much."
- WHY NEED TISSUE ENGINEERING- "AN A.C.L. DOES NOT tear so much as it explodes, often during routine athletic maneuvers — landings from jumps, decelerations from sprints — that look innocuous until the athlete crumples to the ground. After the A.C.L. pulls off the femur, it turns into a viscous liquid. The ligament cannot be repaired; it has to be replaced with a graft, which the surgeon usually forms by taking a slice of the patellar tendon below the kneecap or from a hamstring tendon. One reason for the long rehabilitation is that the procedure is really two operations — one at the site of the injury and the other at the donor site, where the tendon is cut."
- WOMEN AT RISK- "female athletes rupture their A.C.L.’s at rates as high as five times that of males."
- ISSUE HYPOTHETICAL EXAMPLE WOMEN AT RISK- "So imagine a hypothetical high-school soccer team of 20 girls, a fairly typical roster size, and multiply it by the conservative estimate of 200 exposures a season. The result is 4,000 exposures. In a cohort of 20 soccer-playing girls, the statistics predict that 1 each year will experience an A.C.L. injury and go through reconstructive surgery, rehabilitation and the loss of a season — an eternity for a high schooler. Over the course of four years, 4 out of the 20 girls on that team will rupture an A.C.L."
- MORE THAN INJURY-"Each of them will likely experience “a grief reaction,” says Dr. Jo Hannafin, orthopedic director of the Women’s Sports Medicine Center at the Hospital for Special Surgery in New York. “They’ve lost their sport and they’ve lost the kinship of their friends, which is almost as bad as not being able to play.”
- WOMEN AT RISK DUE TO BIOMECHANICS- "“Women tend to be more erect and upright when they land, and they land harder,” he [Steve Marshall, a professor at the University of North Carolina’s School of Public Health, who leads a large A.C.L. study financed by the National Institutes of Health that is following students at the three major U.S. military academies] said. “They bend less through the knees and hips and the rest of their bodies, and they don’t absorb the impact of the landing in the same way that males do. I don’t want to sound horrible about it, but we can make a woman athlete run and jump more like a man.”"
- SERIOUS FEMALE ATHLETE PSYCHE- "JANELLE’ HIGH SCHOOL, St. Thomas Aquinas, is the alma mater of the tennis immortal Chris Evert and the former football star Michael Irvin. It places a high value on attracting and developing young athletes, and on keeping them healthy enough to go on and play in college. “I get more compliance from the boys,” the school’s athletic trainer, Dwayne Owens, told me. “Boys are actually willing to sit if that’s what I tell them. The girls want to get back out there. They want me to tape them up and let them play.” I repeatedly heard similar sentiments from doctors, coaches and others: Girls are more likely to put themselves at risk. If they’ve played through a lot of pain in the past, they may be inured to it."
- USE THIS EXAMPLE IN INTRODUCTION TO GRAB ATTENTION-
- Amy Stedman- "In her junior year in high school, in Brevard, N.C., Parade magazine named her the top high-school-age defensive player in America, “the best of the best.” She was a captain of the U.S. women’s under-19 team, a future star of the women’s national team. She played for Anson Dorrance at U.N.C., and while I was talking to him one day, he pointed out beyond his office door to a gallery where the uniforms of his all-time greats, including Mia Hamm, were displayed. “She would have been one of those jerseys out there,” he said, referring to Amy."
- "But by the time I met her, Amy was 21 and had torn the A.C.L. in her right knee four times. The first time was when she was training for the under-19 World Cup."
- "As Amy walked toward me the first time we met, her right leg was stiff and her whole gait crooked. She moved like a much older woman. If I hadn’t known her history, I would never have believed she had been an athlete, let alone an elite one. She had undergone, by her count, five operations on her right knee. Her mother counted eight, and believed that Amy did not put certain minor cuttings in the category of actual operations. She was done playing. She had been told she would need a knee replacement, maybe by the time she turned 30."
- "Amy told me about her final operation, recalling that when she came out of anesthesia, the surgeon seemed as if he was going to cry. He looked at her in silence for what seemed like a long time, trying to compose himself. Finally, he told her, “Amy, there was nothing in there left to fix.”"
- FEMALE ATHLETE PSYCHE: "That was still Janelle’s mind-set: Rehab hard. Get back on the field. Compete fiercely. And hope not to be injured."
Role of biomechanics in the understanding of normal, injured, and healing ligaments and tendons
http://www.ncbi.nlm.nih.gov/pubmed/19457264
- WHY NEED TISSUE ENGINEERING- "It is also known that a midsubstance anterior cruciate ligament (ACL) tear has limited healing capability, and reconstruction by soft tissue grafts has been regularly performed to regain knee function. However, long term follow-up studies have revealed that 20–25% of patients experience unsatisfactory results."
- WHY NEED TISSUE ENGINEERING- "Well over 100,000 of these procedures are done per year in the U.S. alone [13]. However, long term follow-up studies have revealed that 20–25% of patients experience unsatisfactory results at 7 to 10 years following ACL reconstruction"
- FUNCTION- "Because the primary function of ligaments and tendons is
to transmit tensile forces, experimental studies of the biomechanical
properties of these tissues are generally performed
in uniaxial tension... tensile tests have been performed with the ligament
or tendon insertions to bone left anatomically intact" - HOW TO MEASURE AREA- "developed to measure both the cross-sectional area
and the shape of soft tissues with high accuracy and precision" - FUNCTION- "Additionally, since ligaments and tendons are highly
organized fibrous tissues, their mechanical properties are
directionally dependent (anisotropic)." - FUNCTION-"Mathematical models have been made to describe the viscoelastic
properties of ligaments and tendons." - PROPERTY- "Age-related changes are one biological factor worth discussing"
- FUNCTION- "The properties of ligaments and tendons also can change
with advancing age as well as with activity level" - WHY ACL DOES NOT HEAL- "Unlike extraarticular
ligaments, there exist several well known factors that
limit the ACL from healing [178,179]. The thin synovium
surrounding the ACL, which has been shown to play an
important role in providing a vascular supply to the relatively
avascular ACL as well as to protect it from the harsh
synovial fluid [180], is disrupted and not regenerated
until 1 to 2 months following ACL injury [175,181-183].
Histological examination of the human ACL reveals that
it is also retracted following rupture and that clots formed
are insufficient to fill the open gap" - CURRENT OPTIONS- "Surgical replacements have been done
for a large percentage of patients to help maintain knee
stability [196-200]. Autografts, such as the bone-patellar tendon-bone (BPTB) and hamstring tendons, and allografts
are the graft of choice... 20–25% unsatisfactory results, with complaints
such as knee pain and extension deficits [78,201-204],
and most concerning, many of these cases had progressed
to knee osteoarthritis" - TEST- "To assess the function of the ACL under multiple degree of
freedom (DOF) knee motion, our research center has
developed a robotic/universal force moment sensor (UFS)
testing system since 1993 (Figure 4) [218]. This novel testing
system can control and reproduce the multiple DOF
knee motion [38,40,41,219-221] and is also capable of
applying external loads to knees. By operating in both force
and position control modes, the robot can apply a predetermined
external load to the specimen, such as those
used for the diagnosis of ACL deficiency" - COMPUTER MODELS- "Computational finite element models are also valuable for
studying for the complex function of the ACL and its bundles.
Once such models are validated with experimental
data (e.g., knee kinematics or in-situ forces as determined
using the robotic/UFS testing system [227,228]), they can
be used to calculate the stress and strain distribution in the
ACL, by incorporating its non-uniform geometry (in which
the midsubstance cross-sectional area is one-third that of
the insertions) and its twisting fiber orientation." - TISSUE ENGINEERING COULD LEAD TO BETTER RESULTS- "The use of growth factors, gene
therapy, cell therapy, and biological scaffolds to enhance
healing certainly will result in improved outcomes
[61,242-247]. We believe the ECM-derived bioscaffolds
will play a significant role because it could accelerate the
healing process and establish a bridge between the torn
ends."
The phenotypic responses of human anterior cruciate ligament cells cultured on poly(-caprolactone) and chitosan
http://www3.interscience.wiley.com/journal/117935006/grouphome/home.html
probably only use for background too specific
probably only use for background too specific
- PURPOSE OF THIS STUDY- "The purpose of this study is to evaluate the phenotypic responses of human anterior cruciate ligament (ACL) cells on two biodegradable materials: poly(
 -caprolactone) (PCL) and chitosan"
-caprolactone) (PCL) and chitosan" - CHITOSAN- "Chitosan is a deacetylated product of chitin that is a plentiful polysaccharide found in nature and is safe for the human body. It was reported that this material could accelerate the wound healing and stimulate the macrophage releasing lots of growth factors to promote ECM production"
- PCL- "poly(
 -caprolactone) (PCL) is a synthetic and semi-crystalline linear
-caprolactone) (PCL) is a synthetic and semi-crystalline linear  -polyester and has been used as an implantable material for a long time."
-polyester and has been used as an implantable material for a long time." - FDA APPROVED- "Both PCL and chitosan are biodegradable and have been approved by Food and Drug Administration (FDA)"
- bad results for chitosan adhesion, better for PCL specific numbers in article- "After 4 h of adhesion, cell number on PCL (48,800 � 4100) and chitosan (17,900 � 5300) showed a significant difference... After incubation for 3 days, cell growth was observed on both substrates. The cell number on PCL and chitosan increased to 91,100 � 16,700 and 29,000 � 4100, respectively" (the symbol thing is plus or minus)
- NEED- "Therefore, a substrate with the activity to promote cell adhesion and ECM production is very valuable."
- SUPPORT CHITOSAN AS SCAFFOLD- "These results support the chitosan as scaffold for ACL tissue engineering, which can stimulate ACL cells to synthesize more quantity of FN and TGF
 1 proteins."
1 proteins."
Biomimetic Stratified Scaffold Design for Ligament-to-Bone Interface Tissue Engineering
http://www.ncbi.nlm.nih.gov/sites/entrez
- ABSTRACT- "Biological fixation will require re-establishment of the structure-function relationship inherent at the native
soft tissue-to-bone interface on these tissue engineered grafts. To this end, strategic biomimicry must be incorporated into
advanced scaffold design." - ADVANCES- "Significant advances have thus been
made in the development of ligament- [1-7], tendon- [8-13],
cartilage-[14-24] and bone-like [25-34] tissues by combining
cells and biomaterials along with biochemical and/or biophysical
stimulation" - TISSUE TO TISSUE INTERFACE- "Therefore,
the development of integrated musculoskeletal tissue
systems will require not only the re-establishment of the inherent
structure-function relationship of each type of tissue,
but also the concurrent regeneration of the complex tissueto-
tissue interface." - MULTI-PHASE SCAFFOLD-" It is anticipated that the formation of integrated tissue
systems similar to those observed at the junctions between
orthopaedic soft and hard tissues will require a multi-phased
scaffold which supports the growth and differentiation of
multiple cell types." - PROBLEM WITH TENDON ACL RECONST.- "While
tendon-based ACL reconstruction grafts may restore the
physiological range of motion through mechanical fixation,
biological fixation is not achieved. In the absence of an anatomical
interface, the graft-bone junction exhibits poor mechanical
stability [56-58] and this remains the primary cause
of graft failure" - UNDERSTAND MATERIAL PROPERTIES- "In the paradigm for functional tissue engineering outlined
by Butler et al., [37] significant emphasis is placed on understanding
the material properties of the tissue to be replaced,
as well as quantifying the in vivo strains and stresses experienced
by the native tissue under physiological loading." - 3 REGIONS OF TISSUES IN ACL- "three distinct tissue regions are found at the ACL-bone insertion site: ligament, fibrocartilage, and bone. The fibrocartilage
region is further divided into non-mineralized fibrocartilage
and mineralized fibrocartilage regions" - DESIGN MORE THAN 1 TYPE OF TISSUE NEEDS TO BE ABLE TO REGENERATE- "Thus interface scaffold design
must consider the need to regenerate more than one type of
tissue" - STRUCTURE-FUNCTION PERSPECTIVE
- REGIONAL TENSION- "when the joint is loaded in tension, the deformation
across the insertion site is region-dependent, with the
highest displacement found at the ACL, then decreasing in
magnitude from the fibrocartilage interface to bone" - COW STATS ACL REGION- "bovine ACL-bone interface,
the compressive modulus of the non-mineralized fibrocartilage
region was 0.32 ± 0.14 MPa [71], which is more
than 50% lower than that of the mineralized fibrocartilage
region which averaged 0.68 ± 0.39 MPa [71]. Both of these
values are lower than that of trabecular bone which is reported to be 173 ± 97 MPa in the neonatal bovine model" - FIGURE 1 Biomimetic Stratified Scaffold Design for Ligament-to-Bone Interface Tissue Engineering
- STRATEGY TO ENGINEER MECH. INHOMOGENITY IN SCAFFOLD- "one strategy to engineer controlled mechanical
inhomogeneity on the interface scaffold is by regulating the
distribution and concentration of calcium phosphate on the
scaffold phases." - LAYERED SCAFFOLD- "a stratified scaffold is required
to recapitulate the multi-tissue organization observed at the
native ligament-to-bone interface" - CHALLENGE B/C DIFFERENT TISSUE TYPES IN ACL- "The multi-tissue transition from ligament to fibrocartilage
and to bone at the ACL-bone interface represents a significant
challenge for functional interface tissue engineering
as several distinct types of tissue are observed at this insertion
site." - DIFF. TISSUE TYPES-"supporting the
growth and differentiation of relevant cell populations, must
direct heterotypic and homotypic cellular interactions while
promoting the formation and maintenance of controlled matrix
heterogeneity" - DIFF. TISSUE TYPES- "The interface scaffold must also exhibit mechanical properties
comparable to those of the ligament-to-bone interface. In
addition, the scaffold phases should be biodegradable so that
it can be gradually replaced by living tissue, and the degradation
process must be balanced with respect to the scaffold
mechanical properties in order to permit physiological loading
and neo-interface function." - STRENGTH- "strength of the ligamentous
tissue is crucial to the success of the ACL graft" - FROM OTHER ARTICLE COOPER ET. AL.- "Recently, Cooper et
al. [6] reported on a multi-phased design of a synthetic ACL
graft with a ligament proper as well as two bony regions.
This novel ACL scaffold was fabricated from 3-D braiding
of polylactide-co-glycolide fibers, and scaffold porosity differed
between the bone and ligament regions, with the extended
goal of promoting ACL graft integration within the
bone tunnels. In vitro [7] and in vivo [91] evaluation of this
ACL fibroblast seeded scaffold demonstrated biocompatibility,
healing and mechanical strength in a rabbit model. This
new design represents a significant improvement over single-
phased ACL grafts, and the next step is to address the
challenge of graft integration with bone, by including the
fibrocartilage interface in the ligament scaffold design." - 3 PHASE SCAFFOLD
- tri-phasic scaffold
- "With this scaffold design, a biomimetic
phase-specific cell distribution was established, with osteoblasts
and fibroblasts localized in their respective regions,
while their interaction was restricted to Phase B, the interface
region." - 3 PHASE- "While both anatomic ligament- and bone-like matrices
were formed on the tri-phasic scaffold in vitro and in vivo,
no fibrocartilage-like tissue was observed in the interface
phase through osteoblast-fibroblast co-culture." - OPTIMAL CLINICAL OUTCOME- "The optimal clinical outcome is to have a completely mineralized tissue within the bone tunnel, accompanied by the formation
of an anatomic fibrocartilage insertion on the soft tissue
graft."
Tissue Engineering of the Anterior Cruciate Ligament: The Viscoelastic Behavior and Cell Viability of a Novel Braid–Twist Scaffold
http://www.ncbi.nlm.nih.gov/pubmed/19723437
- OVERVIEW OF STUDY- "In this study we tested novel braid–
twist scaffolds, as well as braided scaffolds, twisted fiber scaffolds and aligned fiber scaffolds, for use as ACL replacements composed of poly(L-lactic acid) fibers. Scaffolds were examined using stress relaxation tests, cell viability assays and scanning electron microscopy." - WHAT IS AN AUTOGRAFT AND WHAT IS AN ALLOGRAFT- "Autografts utilize tissue from the patient and allograft materials are obtained from a cadaver."
- FUNCTION WHAT ACL DOES- "The ACL is a viscoelastic tissue with a time-dependant and load history dependant response to applied forces [10]. This is typically manifested as creep, a change in sample length at a constant stress, or stress relaxation, a decrease in
stress at a constant length. The viscoelastic response of the tissue is typically studied
with creep or relaxation tests at one load or strain level [10]. This behavior is
caused by the arrangement of the collagen fibers in the ligament, interactions between
collagen and other macromolecules in the matrix (such as proteoglycans),
and removal of water from the matrix with applied force." - THEIR TECHNIQUE- "Our scaffold technique (the braid–
twist) is designed to mimic the biomechanical properties and structure of the natural
ligament while providing an environment conducive for cell and tissue growth." - PARAMETERS- "Structural parameters such as braiding and twisting angle were varied in order to optimize
scaffold behavior. Differences in cellular proliferation between these braid–twist
and braided scaffolds were also measured." - THEIR TYPES OF SCAFFOLD- "Braiding and twisting angles were varied for each type of scaffold, yielding a total of 15 types of scaffolds for testing
(6 twisted scaffolds, 3 braided scaffolds and 6 braid–twist scaffolds)." - USE OF MATH MODELS 2.3 MODELING OF MECHANICAL DATA- "The mechanical behavior of the different braid–twist scaffolds were modeled with
a linear viscoelastic model and a quasi-linear viscoelastic (QLV) model. The linear
viscoelastic model was a series of Maxwell models, a combination of a spring and
a dashpot. The equation for the stress at time, t , for a Maxwell model is given in
equation (1):
σ(t) = σ0e−t/τ , (1)
where the stress is noted by σ and the relaxation time is τ . After placing three
Maxwell models in series, the equation for the stress in this system at time t is
given by equation (2):
σ(t) = Xσ0e−t/τx + Yσ0e−t/τy +Zσ0e−t/τz , (2)
where X, Y and Z are the contributions of the yarns, fiber bundles and fibers. The
relaxation times of these parts are τx , τy and τz.
The constants X, Y and Z were the same for each combination of braiding and
twisting angle with four and six turns per inch." - RABBIT ACLS- "Primary patella tendon (PT) fibroblasts from female New Zealand
white rabbits were harvested and cultured as reported earlier" - PROMISE OF REGENERATION OF LIGAMENTS- "In vivo studies with this 3-D braided tissue-engineered ligament (TEL) display
the tremendous promise of this scaffold toward the functional replacement
and regeneration of ligaments [22]." - WHY USE 3-D BRAIDING- "The fibers in the 3-D braiding technique all reinforce
one another, thus increasing scaffold strength; 3-D braiding also creates a network
of interconnected pores to aid in tissue infiltration and cell migration." - WHY USE BIOMATERIAL-" PLLA is a
degradable polymer which allows load to gradually shift from the implant to the
neoligament over time." - GROWTH OF ECM IN FIGURE 9- "growth of extracellular
matrix material on both types of scaffolds over a 28-day period" - HOW TO IMPROVE- "Future work will focus on optimizing the stress relaxation behavior,
investigating braid–twist scaffold porosity and optimizing the mathematical models."
Translational Studies in Anterior Cruciate Ligament Repair
http://www.liebertonline.com/doi/abs/10.1089/ten.tea.2009.0147
- WHY NEED IT-"Recent years have shown a clearer
definition of the clinical problem and established an underlying mechanistic cause of the incapacity of the
anterior cruciate ligament to heal—the premature loss of provisional scaffold in the wound site. These clinical
findings were then translated into a research objective, namely, to replace the missing scaffold with a biomaterial
with appropriate structural and bio-stimulatory characteristics." - WHY NEED IT- "Current estimates of
the prevalence of reported ACL tears range at 4.8% of ambulatory
individuals between 50 and 90 years of age, but it is
very likely that the actual number, including asymptomatic
tears in patients with low demand, is even higher.2,3 The risk
of ACL tears is significantly increased by participating in
particular sports, especially those involving pivoting, and for
women.4–8 ACL tears are serious injuries causing immediate
pain and loss of mobility." - COLLAGEN AS BIOMATERIAL- "Among all biomaterials currently used in tissue
engineering, collagen has a long-standing record as a biocompatible,
biodegradable, and safe material for orthopedic
applications and is the main constituent of the ACL" - COLLAGEN IN COW ACL- "Murray et al. showed that cells from human torn ACL
migrate into a scaffold made from bovine atelocollagen (Fig. 3) and secrete smooth muscle actin, which causes
wound contraction44,45,62 (Fig. 2). ACL fibroblasts retain this
ability also in the ruptured ACL, where they exhibit even
higher outgrowth rates.62" - WHY DOES ACL NOT HEAL- "A translational research approach helped to identify one
potential reason why the torn ACL does not heal: the lack of a fibrin clot that stabilizes the defect and serves as a scaffold
for cell migration and a source for stimulating factors."
reading done let the note taking begin
I read all 8 of the scientific journal articles and found out that one of them really was not that relevant to my topic (so I won't use it). The article from The New York Times Magazine literally made me cry. I guess I felt I have a similar story to several of the young women in the article. I think I may want to forget my questions on whether the treatment will ever be accepted in the US as the standard of treatment and does benefit outweigh cost. I want to incorporate why women are at higher risk for ACL tears instead of those questions. Also I have realized that a few of the articles are on different techniques of creating the artificial ligament, but share common themes of the need for biodegradable material and strength testing. I think I will zone in on when specific technique while using the other articles for background information and such. I will now proceed to blog my notes on the articles (except the one that isn't relevant to my topic).
Monday, October 19, 2009
Anterior cruciate ligament reconstruction: a look at prosthetics - past, present and possible future
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2322926/
Abstract
Abstract
- "history of the use of prosthetics"
- "Carbon Fibre, Gore-Tex and Darcon prosthetics... Leeds-Keio Artificial Ligament and the Kennedy Ligament Augmentation Device (LAD)"
- "(ACL) is the most
frequently injured ligament in the knee" - "poor intrinsic healing ability"
- surgical reconstruction
- "patients who experience ACL injuries
are significantly younger and more active than those
who experience many other orthopaedic injuries. The
need for reconstruction options that exhibit longevity" - primary repairs- fail
- prosthetic replacements- inadequate
- biological tissue autograft- popular
- "ACL anatomy, tissue
composition, biomechanics, and the healing processes.
Unfortunately, to date, no prosthesis has proven itself as
a viable alternative to the patellar or hamstring tendon
autografts, currently used in over 90% of ACL
reconstructions."
- "Bone-patellar tendon-bone (BPTB) and
semitendinosus/gracilis tendon autografts are currently
the most common grafts" - "Both techniques
now offer a high degree of strength and stiffness in the
reconstructed ligament." - PROBLEMS W. PATELLA AND HAMSTRING GRAFT- "Nonetheless, with patellar tendon
autografts, many patients experience impaired function
and significant morbidity at the donor site including
secondary anterior knee pain, patellar tendonitis,
infrapatellar contracture, and patellar fracture.
Likewise, hamstring weakness and saphenous nerve
injury can be seen secondary to hamstring harvest in
semitendinosus/gracilis autograft ACL reconstruction" - PROBLEMS W. DONOR(CADAVER) ACLS- "the use of
allografts is not currently considered advantageous due
to a limited donor tissue supply, delayed biological
incorporation, risks of disease transmission and tissue
rejection."
- history of ACL grafts- 1918 silk sutures fail 3 months
- 1973 PTFE break 1 year
- GRAFTS- "Grafts
(polyethylene, PTFE), typically fixed at both ends, were
the initial focus of synthetic ACL replacement and were
meant to provide stability to the ACL-deficient-knee
until secondary reconstruction procedures gained
popularity (11)." - lig. augmentation- "Similarly, ligament augmentation
devices (polypropylene, polyester) were intended to
provide immediate protection for autogenous tissue
grafts until revascularization was complete and the
ingrown tissue was capable of withstanding local tensile
and compressive forces." - total prosthesis
- no tissue maturation
- long-term -> poor
- scaffold design
- problems- "Problems associated with the biological
incorporation of scaffolds include variability of tissue
in-growth, immature degeneration of the implant and
insufficient maturation of the host tissue resulting in an
inability of the scaffold to withstand inherent
mechanical stresses placed on the ACL."
- carbon fibre prostheses
- 1977
- "migration of carbon wear particles into
the joint space and regional lymph nodes following
implantation of the prosthesis" - coat carbon to solve
- "Surgicraft ABC prosthetic ACL"
- "only 11 of 31 knees (41%) had good results
defined as a Lysholm score greater than 76." - ADVANTAGE DISADVANTAGE TABLE ON P. 31!!!!
- "The Gore-Tex ligament prosthesis is composed of a
single long fiber of expanded polytetrafluoroethylene
(PTFE) arranged into loops. Extensive mechanical
testing has shown that the resulting ultimate tensile
strength is about 3 times that of the human ACL and the
results from cyclical creep tests and bending fatigue
testing seem to identify Gore-Tex as the strongest
synthetic ACL replacement in terms of pure material
stability" - deteriorates over time
- decreasing success rate over years
- "90% success rate at 2 years
versus only a 76% success rate at 3 years or more" - "The Gore-Tex ACL prosthesis is currently FDA
approved for use in patients who have had a failed
autogenous intra-articular graft procedure."
- "The implant is a
composite of four tightly woven polyester strips
wrapped in a sheath of loosely woven velour, designed
to minimize abrasion of the graft and act as a scaffold
for fibrous tissue ingrowth." - failure rate- 31.7% in 50 months
- failure rate- 47.5% in 4 years
- deterioration
- NOT VIABLE
- "a polyester meshlike
structure anchored to the femur and tibia with bone
plugs (24)" - "The implant was considered
sufficiently flexible to be effective with a maximal
tensile strength of approximately 2100 Newtons (N),
which significantly exceeds that of the average young
adults’ natural ACL (about 1730 N)" - ingrowth of unaligned fibrous tissue
- long-term show deterioration
- NOT VIABLE
- "The graft,
composed of a band-like braid of polypropylene, was
originally developed to reinforce the area of pre-patellar
tissue considered to be a weak area of autogenous
patellar tendon grafts." - "Comparisons of the patellar tendon and
semitendinosus/gracilis LAD composite grafts revealed
that the LAD will accept approximately 28% and 45%
of the applied load, respectively (31)." - attached to bone at one end only
- collagen fibers
- "Furthermore, as an intra-articular foreign body, the
LAD has been reported to induce an inflammatory
response characterized by foreign body giant cells and
macrophages in the surrounding tissue." - LACK OF WIDESPREAD USE- NOT GOOD
- "The Ligament Advanced Reinforcement System
(LARS) (Arc-sur-Tille, France) artificial ligament
consists of fibres made of polyethylene terephthalate
(PET)." - knitted structure
- fibers twisted at right angles (90 degrees)
- mimic natural lig. structure
- encourage tissue ingrowth b/c of porosity
- "Thirty-eight
of forty-seven patients suffered from chronic
ruptures of the ACL, while nine others presented with
acute or subacute ruptures at a mean follow-up of 21.9
months. Six patients had previously had an
unsuccessful ACL reconstruction." - Scales to test knees- Tenger activity scale, telos radioactive stress system
- "no patients returned to pre-injury activity levels"
- chronic instability
- Lysholm score
- RISK OF RUPTURE
- "Permanent synthetic prostheses are capable of
duplicating the mechanical and structural properties of
the ACL. However, they generally tend to lose strength
with time. Tissue-based or tissue-aided implants offer
the additional possibility of the restoration of normal
joint kinematics while the mechanical behaviour of
these implants is expected to improve over time as tissues are remodelled within the knee" - "must also degrade at a rate similar to that
of tissue ingrowth. Accordingly, the ACL scaffold
should lose its mechanical integrity while allowing the
remodelled tissues to gain strength and accept an
increasing amount of the mechanical demands placed
on the ACL. Current research into this novel tissueengineering
approach has focused on seeding either
collagen-based scaffolds or synthetic biodegradable
polymers with a variety of different cell types." - "rabbit fibroblasts on skin and ACL scaffolds"
- "As an alternative to the scaffolds made of nondegradable
polymers, investigators have begun to
examine biodegradable materials that would provide
immediate stabilization to the repaired ligament but
would also act as a scaffold for the ingrowth and/or
replacement by host cells. Cao et al. described the
generation of neo-tendons in a nude mice model by
implanting polyglycolic acid (PGA) scaffolds seeded
with bovine tendon fibroblasts in the subcutaneous
space of athymic mice" - PGA scaffolds
- bone marrow stomal cells
- "The future of tissue engineering may also require a
significant contribution from cell-specific growth
factors influencing the maturation and homeostasis of
the healing response of ligament tissue." - "the optimal activity of each growth factor"
- "computer-assisted surgery in an attempt
to reduce the incidence of graft failure" - "the use of computer-assisted
ACL reconstruction may lead to similarly dramatic
improvements in technical and functional outcomes"
- past 30 years
- "Most of the grafts that have been
developed to date have failed due to unsatisfactory
long-term physiologic and functional performance.
Most permanent ACL prostheses are prone to creep,
fatigue, and mechanical failure within several years
after implantation (40). Tissue ingrowth scaffolds and
ligament augmentation devices require further
refinement to provide effective mechanical support
while avoiding stress-shielding of the host tissue. In
view of these factors, prosthetics are not widely used
today in ACL reconstruction, and autogenous tissue
grafts remain the gold standard used by the majority of
surgeons." - FUTURE- "Advances in
tissue engineering combined with developments in
molecular biology and gene therapy may couple with
the rapid gains in computer-assisted surgery to provide
improved options for the ACL-deficient knee, with a
greater potential to restore its pre-injury state."
Fiber-based tissue-enginered scaffold for ligament replacement: design consideration and in vitro evaluation
I am going to title each of the posts by the title of the article to make it easier for me to find notes on each article. P.S. the link for this article is posted in an older post.
Abstract
Abstract
- ACL- "most commonly injured ligament of the knee"
- "150,000 ACL surgeries performed annually in the US"
- "biodegradable, tissue-engineered ACL graft"
- "construct architecture, porosity, degradability, and cell source"
- "polymeric fibers of polyactide-co-glycolide 10:90"
- "three-dimensional braiding technology"
- "over 250,000 patients each year diagnosed with a torn ACL"
- "current treatment... bone-patellar, tendon-bone and hamstring-tendon"
- "donor site related problems"
- "commercially available synthetic ACL grafts... Gore Tex prosthesis, the Stryker-Dacron ligament, and the Kennedy ligament augmentation device (LAD)... long-term clinical
- Def. tissue eng.- "Tissue engineering may be defined as the application of biological, chemical, and engineering principles toward the repair, restoration, or regeneration of living tissues using biomaterials, cells, and factors alone or in combination"
- Ideal- "The ideal ACL replacement scaffold should be
biodegradable, porous, biocompatible, exhibit sufficient
mechanical strength, and able to promote the formation
of ligamentous tissue." - Architecture
- "Scaffolds developed within these
pore size ranges will encourage tissue ingrowth, capillary
supply, and improve the quality of anchorage in bone
tunnels." - "increases the overall surface area
for cell attachment, which in turn can enhance the
regenerative properties" - Biodegradable materials
- no foreign body reaction
- PLGA fibers
- ACL- 3 areas where fibers arranged- "anteromedial, posterolateral,
and intermedial" - Objective-"design a scaffold
that would provide the newly regenerating tissue a
temporary site for cell attachment, proliferation, and
mechanical stability." - Cell source and response
- scaffold biocompatibility
- braiding, PLAGA 10:90
- Architecture- pore diameter, porosity, surface area
- Mechanical properties
- tensile strength
- load as a function of braiding angle
- cells and cell culture
- scaffold in vitro evaluation
- cell growth
- scanning electron microscopy
- "effects of braiding geometry ib the linear density, mode pore diameter, median pore
diameter, surface area, braiding angle, and porosity of
the scaffolds can be derived from Table 1." - surface area
- braiding angle
- mechanical properties
- "differ in strength due to differences in strain rate
and geometry" - "cell adhesion and spreading on the braided scaffold"
- primary rabbit ACL cells
- "primary ACL cells clustered and grew in small groups
on the 3-D scaffold" - spread across fiber- Fig. 4
- cell migration and attachment- Fig. 5
- mouse 8 days- Fig. 6
- rabbit 8 days- Fig. 7
- Advantages- "controlled porosity
and pore diameter to encourage tissue infiltration
throughout the scaffold, which are lacking in most
ACL artificial implants. The 3-D braiding system
allowed for custom production of scaffolds with
mechanical properties similar to those of natural
ACL tissue in order to overcome issues of stress
shielding during tissue ingrowth. In addition, the
intertwining of the fibers within the 3-D braid prevents
total catastrophic failure of the scaffold due to a small
rupture." - manipulate braiding angle to inc. or dec. porosity and mode pore diameter
- optimal pore size
- "lower limit pore size of 100 mm
[24,25]. A minimum pore size of 150 mm has been
suggested in the literature for bone and 200–250 mm
for soft tissue" - "optimal pore diameters of
100–300 mm needed for in vivo tissue ingrowth" - PREVIOUSLY IN PAST- "Previous ligament prostheses have been made of
flexible composites consisting of fibers that have been
woven or braided into structures [11,14]. These scaffolds
performed well for a short period after implantation,
while the long-term results have been poor [11,14]. These
composite structures were limited by poor tissue
integration, poor abrasion resistance, and fatigue failure
[11,14]." - regnerate tissue between pores
- structural properties
- "ultimate tensile strengths ranged
fromB100 to 400 MPa" - circular better- "the circular
braid geometry showed a significant increase in maximum
tensile load. The 3-D circular fibrous scaffold was
able to withstand tensile loads of 907N (SD7132 N),
which was greater than the level for normal human
physical activity that is estimated to range between 67
and 700N [40–42]." - crimp geometry- "mimic stiffness of natural ligament"
- pore diameters- "167 and 260 um... tissue ingrowth"
- "biocompatibility of scaffold"
- rabbit slower growth than mouse
- mouse not used in future studies
- WHY NEED TISSUE ENG.- "ACL tissue engineering is need because of past
failures in ligament reconstruction using prostheses." - "parameters that must be addressed
to produce a biocompatible tissue-engineered ligament
replacement" - NIH grant
Loads of Information
I have gathered eight articles from scientific journals on my research topic. I have looked through the abstracts of each, and they all seem pretty relevant. Most of the articles were found using PubMed (including the article that I mentioned in a previous post). I also have one article from the New York Times Magazine that is relevant to my topic. So far I have only read, highlighted, and took notes on two of the articles. I will give each article it's own post in an effort to keep this semi-organized.
Thursday, October 15, 2009
More Specific Questions
I determined that I am researching tissue-engineered scaffold for ACL replacement. My core questions are below.
In addition to the questions above, I have a few questions that I will bring up in my introduction or conclusion that can be deemed more abstract questions to contrast with the concrete questions above.
CORE
- How is it made? What are the components?
- Will it be as strong as a transplant ACL?
- How does it work and hoe can it be improved?
In addition to the questions above, I have a few questions that I will bring up in my introduction or conclusion that can be deemed more abstract questions to contrast with the concrete questions above.
- Will it ever be accepted in the US as a standard method of treatment?
- Is the cost of full development greater than the possible benefit?
- Why is it important to develop artificial tissue?
CORE
- components
- strength
- how does it work
- how can it be improved
- ever accepted in US as standard treatment
- why develop it
- does benefit outweigh cost
Wednesday, October 14, 2009
ACL
I think I want to research the ACL. From an engineering perspective, the artificial tissue being worked on that could be implanted during surgery. These tissues may reduce healing time. I also want to know why the proportion of female athletes who get ACL tears is much higher than in male athletes. Some claim it is the difference in the quadracep to hamstring strength ratio in the quad. Women have weaker quads than hamstrings, whereas men's quads and hamstrings are about equal in strength.
I have a pretty cool article from PubMed Plus about an artificial ligament involving scaffolding that could be used in ACL reconstruction.
http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6TWB-4CVV79T-1&_user=489256&_coverDate=05%2F31%2F2005&_rdoc=1&_fmt=&_orig=search&_sort=d&_docanchor=&view=c&_acct=C000022721&_version=1&_urlVersion=0&_userid=489256&md5=c3c3a23aced81c1196f3f38ac03280ae
You may have to be on the PennNetwork to read the article. It's abstract is relatively interesting. It really explains how many people are getting this debilitating injury. The article describes the overall situation as well as the specific designs of the tissue scaffolding. I do not know if the topic is too specific or not but we'll go over it tomorrow. To make it more broad I could go into all the articificial knee carilage and ligaments being developed.
If I pick this as my final topic, it will be pretty personal for me knowing what I have been through and the number of people I know who have endured the same thing. One second led to essentially one year of rehabilitation.
Some questions I have are

http://biomed.brown.edu/Courses/BI108/BI108_2004_Groups/Group06/Group6project/Graphics/Therapy/ACL_tear.jpg
I have a pretty cool article from PubMed Plus about an artificial ligament involving scaffolding that could be used in ACL reconstruction.
http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6TWB-4CVV79T-1&_user=489256&_coverDate=05%2F31%2F2005&_rdoc=1&_fmt=&_orig=search&_sort=d&_docanchor=&view=c&_acct=C000022721&_version=1&_urlVersion=0&_userid=489256&md5=c3c3a23aced81c1196f3f38ac03280ae
You may have to be on the PennNetwork to read the article. It's abstract is relatively interesting. It really explains how many people are getting this debilitating injury. The article describes the overall situation as well as the specific designs of the tissue scaffolding. I do not know if the topic is too specific or not but we'll go over it tomorrow. To make it more broad I could go into all the articificial knee carilage and ligaments being developed.
If I pick this as my final topic, it will be pretty personal for me knowing what I have been through and the number of people I know who have endured the same thing. One second led to essentially one year of rehabilitation.
Some questions I have are
- How does it work?
- Why is it important?
- When will it be used in the US as a standard method of treatment?

http://biomed.brown.edu/Courses/BI108/BI108_2004_Groups/Group06/Group6project/Graphics/Therapy/ACL_tear.jpg
Thursday, October 8, 2009
research
What topic should I do for a science research topic? I really do not know. Big things like what cause certain diseases can be pretty complicated. In my writing seminar the other day we watched a clip about how a baby boy got a heart transplant that did not match his blood type. The baby did not reject the heart because his immune system was not fully developed yet. His blood did not yet have antibodies. One would think that doing such an operation could be more harmful than waiting for a proper match, but it ended up working out. That's a pretty cool feat of science I must say. Although this would probably never happen on the large scale in the US due to regulations. The operation was performed quite a few years ago now and the boy is still okay. The link to the news story is below (the clip we watched was from 60 minutes).
http://www.cbsnews.com/stories/2004/03/29/60minutes/main609225.shtml

http://www.cbsnews.com/stories/2004/03/29/60minutes/main609225.shtml

Analyze
Basically any structure can be analyzed on different length scales. As seen from today's recitation dresses, flowers, oranges, computers, buildings, computers, etc. can all be examined in terms of their components. I thought it was pretty interesting how many people chose to relate the structure that they were analyzing to the human body. If you think about it the human body can go from DNA to nucleus to cell to tissue to organ to organ system to body (with tons of other components in between). Even I related my structure, the napkin, to skin without thinking about the fact that this is introduction to bioengineering. It was only after the presentations today that I realized comparing my structure to a part of the human body makes a firmer relation to the field of bioengineering.

http://www.sbceo.k12.ca.us/~impact2/TeachnetArchives/projects/hamner/karen_hamner_body_sys/frontleft.jpg

http://www.sbceo.k12.ca.us/~impact2/TeachnetArchives/projects/hamner/karen_hamner_body_sys/frontleft.jpg
Friday, October 2, 2009
Skin
A napkin is like skin. The scales of the napkin (napkin, layers of napkin, dimples in napkin) can be compared to the scales of the skin (skin, layers of skin, pores in skin). The analogy is quite simple. Skin covers the human body, has layers (epidermis, dermis, hypodermis), and has pores for sweat. Skin covers practically the entire human body. The layers provide for durability and protection, almost like the layers of the napkin. The pores allow for sweat to be released, like the dimples in a napkin allow for extra absorption. The napkin can entirely cover a spill, its layers contribute to the whole, and the dimples allow for more absorption. The form of each of these structures related to the function.

http://www.web-books.com/eLibrary/Medicine/Physiology/Skin/skin01.jpg

http://www.web-books.com/eLibrary/Medicine/Physiology/Skin/skin01.jpg
Napkins
Napkins. They seem pretty simple, not too many "parts." They have components though. If you can tell by now the structure I am analyzing is the napkin. A napkin is "a square piece of cloth or paper used at a meal to wipe the fingers or lips and to protect garments, or to serve food on" according to the dictionary on my MacBook Pro.
The first length scale is the napkin (which has dimensions of 6.25 by 4.5 inches and a depth of maybe 2 millimeters). The next length scale is the layers of the napkin (the napkin has three layers 6.25 by 4.5 inches, 6.25 by 3.5 inches, and 6.25 by 3.5 inches). The final length scale is the dimples in the napkin (maybe like 2 millimeter squares).
This idea was spurred as I was eating lunch at Hill with some friends. I was trying to think of something to analyze for this blog and the structure was literally in my hand. It's so simple, but still can be measured with different length scales. Sure a napkin, may be less impressive than a building, bricks, and mortar, but it can be analyzed in the same way. I saw the napkin while eating an orange. I discovered it could be measured with different scales as I thought about it. I analyzed the various components of a napkin and described it's physical characteristics.
A napkin has to be able to absorb things like water. It can't be too thick though, then it would be a sponge. It has to be soft enough for a person to wipe their mouth with. It can't be rough like sandpaper. It has to have layers for the absorption to work. It can't be too large or too heavy. It can't be like a towel. It has to be durable, more so than a tissue. Sometimes people use napkins to wipe tables. The individual dimples in the napkin work to improve the absorption and increase the 3-D surface area to absorb more liquid.
The first length scale is the napkin (which has dimensions of 6.25 by 4.5 inches and a depth of maybe 2 millimeters). The next length scale is the layers of the napkin (the napkin has three layers 6.25 by 4.5 inches, 6.25 by 3.5 inches, and 6.25 by 3.5 inches). The final length scale is the dimples in the napkin (maybe like 2 millimeter squares).
This idea was spurred as I was eating lunch at Hill with some friends. I was trying to think of something to analyze for this blog and the structure was literally in my hand. It's so simple, but still can be measured with different length scales. Sure a napkin, may be less impressive than a building, bricks, and mortar, but it can be analyzed in the same way. I saw the napkin while eating an orange. I discovered it could be measured with different scales as I thought about it. I analyzed the various components of a napkin and described it's physical characteristics.
A napkin has to be able to absorb things like water. It can't be too thick though, then it would be a sponge. It has to be soft enough for a person to wipe their mouth with. It can't be rough like sandpaper. It has to have layers for the absorption to work. It can't be too large or too heavy. It can't be like a towel. It has to be durable, more so than a tissue. Sometimes people use napkins to wipe tables. The individual dimples in the napkin work to improve the absorption and increase the 3-D surface area to absorb more liquid.
Parts and Functions
Parts are concrete. Functions are abstract. In recitation I attempted to draw a water bottle, a USB drive, and a chalk holder without looking at the paper I was drawing on. The results: images that looked nothing like the actual things I was trying to portray. Sure there might have been some similar shapes, but far from any accurate drawing. No scale, no symmetry, no concrete similarities. If I showed the pictures to someone else, they would have no idea what that object was. I think the more patience you have the more "in the zone" you can be. I have little patience with anything artistic, but I'm sure if I was locked in a room for an hour and had to come up with a drawing of something without looking at it I could do it.
I liked the "thinking without seeing" exercise more than the "seeing without thinking" one. When I started my gozinto diagram for a bicycle I went from big picture to little picture. I ended up with a whooping twenty-six sub-components, sub-sub components, up to sub-sub-sub-sub-sub components all together. Once I did the diagram again with only 6 components I thought of the essential elements that make up a bike: frame, wheels, handlebars, gears, brake, and tires. Notice that does not include pedals or a seat (opps). When drawing a diagram of functions a bike should perform I thought of four: stable with motion, steering system, support person, and speed control. I thought of these and then thought of parts that correspond to each of these functions, such as shock absorption, handlebars, frame, and brake, gears, and pedals, respective to the above functions. I think the functions are more important than the parts, but the parts are needed for the functions.
I liked the "thinking without seeing" exercise more than the "seeing without thinking" one. When I started my gozinto diagram for a bicycle I went from big picture to little picture. I ended up with a whooping twenty-six sub-components, sub-sub components, up to sub-sub-sub-sub-sub components all together. Once I did the diagram again with only 6 components I thought of the essential elements that make up a bike: frame, wheels, handlebars, gears, brake, and tires. Notice that does not include pedals or a seat (opps). When drawing a diagram of functions a bike should perform I thought of four: stable with motion, steering system, support person, and speed control. I thought of these and then thought of parts that correspond to each of these functions, such as shock absorption, handlebars, frame, and brake, gears, and pedals, respective to the above functions. I think the functions are more important than the parts, but the parts are needed for the functions.
Sunday, September 27, 2009
Bioengineering: A Problem or A Solution
Bioengineers spend tons of money researching, developing, and innovating health care technologies. Sure the end result may be a better drug, device, or tissue, but at what cost is it really at? It's obvious that bioengineers contribute to the raising costs of health care through the development of new technologies. They are part of the problem. Although, along with new technologies comes with reducing the cost of the older ones. So basically what I'm saying is bioengineers make new treatments more expensive, but more traditional treatments more affordable.
This may seem different. For bioengineers to be a part of the solution for reducing health care costs, they have to work backwards and forwards at the same time. In other words, bioengineers have to continue to work on new technologies (better drugs, imaging, etc), while also making existing things like a x-ray machines better and cheaper. This is a hard balance for anyone to do. Engineers want to go forwards, not backwards. The end goal here is to reduce health care costs, because the fanciest newest 3-D brain scan is practically useless if no insurance company will approve a test using that.

http://www.ny3d.org/3D_brain_Scan.jpg
This may seem different. For bioengineers to be a part of the solution for reducing health care costs, they have to work backwards and forwards at the same time. In other words, bioengineers have to continue to work on new technologies (better drugs, imaging, etc), while also making existing things like a x-ray machines better and cheaper. This is a hard balance for anyone to do. Engineers want to go forwards, not backwards. The end goal here is to reduce health care costs, because the fanciest newest 3-D brain scan is practically useless if no insurance company will approve a test using that.

http://www.ny3d.org/3D_brain_Scan.jpg
the government has a plan?
Everyone in the US has heard something about health care reform. People heard about it in the months leading up to the presidential election in November 2008, and people have been hearing about it all summer as attempts at reform get twisted into things that barely resemble the initial plan. Last fall I wrote quite a long paper and participated in a debate about Obama's proposed health care plan. I will only focus on the technology aspect of it here. Essentially the common theme among business, education, and government is the recognition of the need for digital health records. The site tells of the nation's progress and lists all of these vague goals in the realm of health care. I am bias on this issue and believe that all American citizens should be given health insurance, but I can still criticize the government's plan.
Eventually there could possibly be a cap on health care spending. There could be a rationing of which technologies are used to treat which patients. How can the government create a policy listing which patients are the priority and which are secondary? Creating clear cut boundaries is difficult in medicine. There are always exceptions to the rule. Not giving a healthy person with a history of cancer routine scans could make it too late before doctors find the tumor. Not giving an athlete an MRI could make them play with an injury and destory their entire knee. Ethical decisions are difficult to make and broad policies can leave people behind.
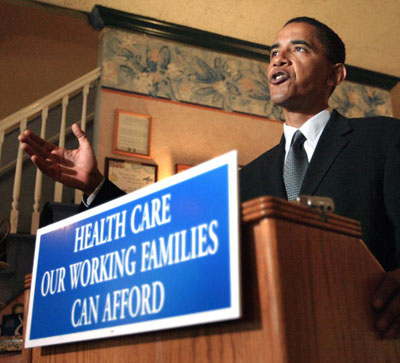
http://abhisays.com/wp-content/uploads/2009/09/obama_healthcare.jpg
http://www.healthreform.gov/
Eventually there could possibly be a cap on health care spending. There could be a rationing of which technologies are used to treat which patients. How can the government create a policy listing which patients are the priority and which are secondary? Creating clear cut boundaries is difficult in medicine. There are always exceptions to the rule. Not giving a healthy person with a history of cancer routine scans could make it too late before doctors find the tumor. Not giving an athlete an MRI could make them play with an injury and destory their entire knee. Ethical decisions are difficult to make and broad policies can leave people behind.
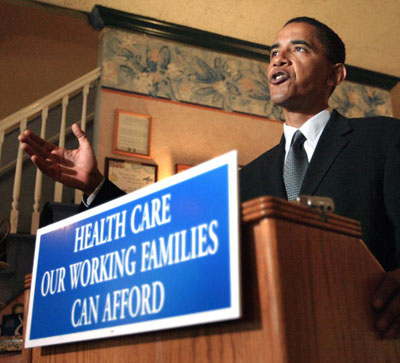
http://abhisays.com/wp-content/uploads/2009/09/obama_healthcare.jpg
http://www.healthreform.gov/
claims, claims, claims (business and education)
As health care technology advances, the older health care technologies become cheaper. Let's take for example an x-ray versus an MRI. The x-ray at the time it was first introduced was a big deal. You could see bone structure. Now MRIs enable easy viewing of bones, muscles, ligaments, etc. X-rays now are cheap (maybe a few hundred dollars- cheap relative to the medical imaging world). MRIs cost thousands of dollars. But because of the advancement x-rays are cheaper and better imaging is out there if needed.
I found a few websites making different claims on how to reduce health care costs. One site talks about how digital data entry and insurance claims entry machines will reduce health care cost. The thing is that the site is a PR log and the article was most likely written by a company representative of E*Healthline.com, which is making such a technology. The article has random statistics that make the information system seem like such a necessity. You have to remember the bias of the source. I kind of believe that digital records will reduce costs, but I did beleive that before I read the article.
Another site mentions how health information technology, individual ability of a patient to research home care, digital health databases, and prescribing medication digitally from the doctor directly to the pharmacy. The site is a ".com" so some sponsors most likely influenced this article. There is no concrete evidence presented in the article either, but I still think that digital databases for records will reduce cost. I am skeptical about the other claims, although they are logical, because they have no facts in the article.
A different website mentions a digital health records database as well as a way to evaluate new technologies in terms of their net gain. The health records database seems like a good thing. The article did not really provide numbers on the benefits of a digital system, but it seems to be a general conclusion that it will reduce costs. The implication of grading technologies in terms of net gain can be difficult. How can you say doing this procedure has risks (like death), but it has benefits (like cutting someone's recuperation time by six months)? I agree that evaluation could lower costs, but how many technologies would never be improved if the world thought that way. It's a tricky game. The site is educational and from the University of San Francisco. It just evaluates a paper that a professor wrote in 2007, so it's tech-saviness is off, while the ideas remain the same. It kind of plugs the university a little more than the topic of reducing costs.

http://origin.arstechnica.com/articles/culture/electronic-health-records.media/Immune_auto.png
http://www.prlog.org/10198630-ehealthline-reduces-health-care-administrative-cost-while-increasing-efficiency.html
http://www.howtodothings.com/health-fitness/how-information-technology-can-reduce-the-cost-of-health-care
http://news.ucsf.edu/releases/better-review-of-new-technology-is-needed-to-reduce-health-costs/
I found a few websites making different claims on how to reduce health care costs. One site talks about how digital data entry and insurance claims entry machines will reduce health care cost. The thing is that the site
Another site mentions how health information technology, individual ability of a patient to research home care, digital health databases, and prescribing medication digitally from the doctor directly to the pharmacy. The site
A different website mentions a digital health records database as well as a way to evaluate new technologies in terms of their net gain. The health records database seems like a good thing. The article did not really provide numbers on the benefits of a digital system, but it seems to be a general conclusion that it will reduce costs. The implication of grading technologies in terms of net gain can be difficult. How can you say doing this procedure has risks (like death), but it has benefits (like cutting someone's recuperation time by six months)? I agree that evaluation could lower costs, but how many technologies would never be improved if the world thought that way. It's a tricky game. The site

http://origin.arstechnica.com/articles/culture/electronic-health-records.media/Immune_auto.png
http://www.prlog.org/10198630-ehealthline-reduces-health-care-administrative-cost-while-increasing-efficiency.html
http://www.howtodothings.com/health-fitness/how-information-technology-can-reduce-the-cost-of-health-care
http://news.ucsf.edu/releases/better-review-of-new-technology-is-needed-to-reduce-health-costs/
Saturday, September 26, 2009
Newer, Better, Cheaper? (10 ways)
Technology can theoretically reduce health care costs. There are a few different specific technologies that can reduce health care costs.

http://evolutionary-research.net/science/intro/the-engine-of-evolution/figures/DNA-DoubleHelix-ImgLibPDB-1bna_prepi_4.gif
- Digital health record databases (more efficient than paper records)
- Automated "check-ups" where the results are sent to your doctor (fewer doctor visits)
- Improved preventative medicine programs (tips and schedules of what to do and what not to do to prevent sickness and chronic conditions)
- Digital ER waiting room evaluation to see if perhaps sending a patient to a clinic is a better option (save money from unnecessary ER visits)
- Giving patients with chronic conditions monitoring systems that could send updates to their physicians (fewer doctor visits)
- Improved virtual reality training for medical students (cheaper than actual training)
- Improved discharge procedures for patients in hospitals (give them individualized programs that can be uploaded onto smart phones)
- Devices that can decrease healing time (decrease doctor visits, less cost)
- Cheaper diagnostic testing for diseases (quicker results, faster treatment is given leads to less treatment needed)
- Genome analysis of a newborn to know ways to avoid diseases they may be prone to

http://evolutionary-research.net/science/intro/the-engine-of-evolution/figures/DNA-DoubleHelix-ImgLibPDB-1bna_prepi_4.gif
Friday, September 25, 2009
what's the deal with the obsession with antibacterials
Random topic, I know. I am reading Genome: The Autobiography of a Species in 23 Chapters by Matt Ridley for my writing seminar, and in one chapter it says that as most scientists know that "our immune sysems are set up in such a way that they 'expect' to be educated by soil mycobacteria early in childhood; when they are not, the result is an unbalanced system prone to allergy" (Ridley, 1999). So the debate is I guess for parents of young children whether to let the immune system develop properly and run the risk of catching some virus at the playground or reduce the risk of catching that virus and possibly making your kids have allergies. I am not anti-purell or something like that, but I do not know what side to pick. Is society as a whole becoming too afraid of germs and is this leading to more sensitive immune systems (allergies, asthma, etc.)? Or are we picking the lesser of two evils? This ethical debate worries me.

https://blogger.googleusercontent.com/img/b/R29vZ2xl/AVvXsEh7FjMAhhinE72IshnbLyo08hPqb0OeXiZnNcmyE4tBSEipMT9HWEc8RKUDUGz8_OnQPyeX1s6hzenVPUpR1sTC3gY5cWW98IvwylsENN7j-hP8gFGBAWc5KKjyhQed4GT0D7EeuTVV_MTX/s400/purell-at-staples-3-4-09.jpg

https://blogger.googleusercontent.com/img/b/R29vZ2xl/AVvXsEh7FjMAhhinE72IshnbLyo08hPqb0OeXiZnNcmyE4tBSEipMT9HWEc8RKUDUGz8_OnQPyeX1s6hzenVPUpR1sTC3gY5cWW98IvwylsENN7j-hP8gFGBAWc5KKjyhQed4GT0D7EeuTVV_MTX/s400/purell-at-staples-3-4-09.jpg
Individual Vs. Community
Health is on an individual level. A person can be healthy (not sick, not obese, not injured), while living in an unhealthy community. Public health is more of an overall entity. It deals more on the overall scale from the community, to the region, to the country, to the world. A public health concern deals with things like smoking. Governments come up with public health policies to attempt to make people healthier overall. Individuals can have poor health in a community with overall good health and vice versa.
Obviously, doing things that impact public health can have an impact on more people that doing things that are in the interest in an individual's health. Providing clean drinking water to the more than one billion people who lack access to that is a public health initiative. An individual going to the doctor to get medicine for a respiratory infection is a personal health issue.

http://www.health.state.nm.us/PHD/Dist3/Graphics/PublicHealthFamily.jpg
Obviously, doing things that impact public health can have an impact on more people that doing things that are in the interest in an individual's health. Providing clean drinking water to the more than one billion people who lack access to that is a public health initiative. An individual going to the doctor to get medicine for a respiratory infection is a personal health issue.

http://www.health.state.nm.us/PHD/Dist3/Graphics/PublicHealthFamily.jpg
what's happened and what will happen
The "Greatest Engineering Achievements of the Twentieth Century" and the "Grand Challenges for Engineering" are so broad that they basically say everything that was ever done was a great feat and everything that will be done will be a challenge. People can definitely try to classify most all accomplishments under one of the twenty categories presented in the list of achievements. As can any challenge be twisted to fit into the categories of the "grand challenges."
Electronics and the Internet are the two biggest achievements that my generation cares about. People around my age basically used a computer since grade-school and the internet since around the same time. Now most people use laptops, ipods, digital cameras, and most recently smart phones. The electronic industry is key in helping define my generation. The internet has created an entire community as well as improved instant communication with anyone anywhere. Networking sites ease communication among far away friends and family members.
Contrasting with what already happened (and is continuing to change as I type this entry), is what will happen and why my generation cares. Securing cyberspace and making solar energy economical are what young people probably care about the most out of all of the challenges. Cyberspace is expanding all the time. More information is available, and with that more viruses are created. If eventually (and I hope this happens within the next few decades) all health care files become digital a much more security will be needed to make it safe. I guess that issue kind of overlaps with advancing health informatics, but if you tell the average eighteen year old what health informatics is odds are they won't care. Solar energy is also an important issue. As we all know or just constantly deny in some cases, the world oil supply is diminishing. Conventional oil used for heating and transportation will become drastically too expensive in the next decades. Natural gas is also a limited resource. People are becoming increasingly concerned with "going green," and they are realizing that fossil fuels are not renewable resources. Making solar energy more economical will be necessary in the future. These days young people have a greater sense of the natural environment than they did years ago.

http://www.sedonawildflowerinn.com/images/going%20green.jpg
Electronics and the Internet are the two biggest achievements that my generation cares about. People around my age basically used a computer since grade-school and the internet since around the same time. Now most people use laptops, ipods, digital cameras, and most recently smart phones. The electronic industry is key in helping define my generation. The internet has created an entire community as well as improved instant communication with anyone anywhere. Networking sites ease communication among far away friends and family members.
Contrasting with what already happened (and is continuing to change as I type this entry), is what will happen and why my generation cares. Securing cyberspace and making solar energy economical are what young people probably care about the most out of all of the challenges. Cyberspace is expanding all the time. More information is available, and with that more viruses are created. If eventually (and I hope this happens within the next few decades) all health care files become digital a much more security will be needed to make it safe. I guess that issue kind of overlaps with advancing health informatics, but if you tell the average eighteen year old what health informatics is odds are they won't care. Solar energy is also an important issue. As we all know or just constantly deny in some cases, the world oil supply is diminishing. Conventional oil used for heating and transportation will become drastically too expensive in the next decades. Natural gas is also a limited resource. People are becoming increasingly concerned with "going green," and they are realizing that fossil fuels are not renewable resources. Making solar energy more economical will be necessary in the future. These days young people have a greater sense of the natural environment than they did years ago.

http://www.sedonawildflowerinn.com/images/going%20green.jpg
Subscribe to:
Posts (Atom)



